Diagnosing and Treating Dysthymia in Children: When Depression is Chronic at an Early Age

When I was finally diagnosed with depression at age 27, after twenty years of suffering from one type of depressive disorder or another, it was because I was going through a major depression at that particular time. It was only the third major depression I had experienced, and all three had occurred after the age of twenty. For all their ferocity, however, I don’t feel that the major depressions did the most damage to my social life, the direction my life took and my psyche. Without question, that honor is reserved for the dysthymia that had been a part of my life, and a part of me, since I was seven.
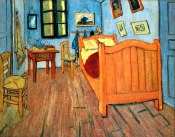
A few years ago, my mother found a picture of me as a baby crawling on the grass. For days, I couldn’t figure out what was so odd about the picture. It finally dawned on me that I was grinning in it, and with the exception of school pictures, I had never seen a photo of myself with anything more than a tentative half-smile. For the most part I looked serious, detached and sometimes, sad.
The psychiatrist who first told me, “I believe that you’re suffering from depression” might have been a bit surprised at how relieved I was. But for me, the diagnosis was a relief. I had known most of my life that something was wrong with me. I was thrilled that this something had a name and could be treated.
My psychiatrist felt it was clear that I had been suffering from depression, in one form or another, since I was a child. It may seem hard to believe that someone could go undiagnosed for so many years, but there were a couple of factors at work. The first was that I grew up in the 1960s and 70s. No one believed back then that children could suffer from depression. My parents did know that something was wrong with me, but they had no idea what it was or what to do. More importantly, however, my depression went unnoticed because I suffered from dysthymic disorder, not major depression.
Major depressive disorder (MDD) and Dysthymic Disorder (more commonly known as dysthymia) do have a lot in common. Both are marked by a low mood, low self-esteem, fatigue or low energy, indecisiveness and hopelessness. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) “Dysthymic Disorder and Major Depressive Disorder are differentiated based on severity, chronicity and persistence.“
In other words, MDD and dysthymia are like rain storms. Both of them drop water from the sky. But if major depression is like a violent thunderstorm, like a thunderstorm it usually passes fairly quickly (although it may seem like an eternity). Dysthymic disorder is like a steady drizzle under a gray sky that goes on and on for days.
Dysthymia is considered early onset dysthymic disorder (EODD) when the symptoms begin before the age of 21. Unfortunately, EODD can be very tricky to spot. After all, if a child has had EODD from an early age, before her personality has been fully formed, how does she (or her parents) know that she suffers from a depressive disorder?
But diagnosis and treatment of EODD is absolutely essential. A child who grows up under the influence of a depressive disorder is going to be at a tremendous disadvantage, not to mention how miserable his childhood is going to be.
Even if I had suffered from major depressions during my childhood, they would not have as much damage as the dysthymia. The drizzle and gray sky that went on day after day, eroding my sense of self and keeping me from being anything other than a spectator in life, was the real devastating force. And under that gray sky I made a lot of important decisions that set me on certain paths: what interests to develop, what type of friends to choose, how to prioritize school and play, where to go to college, what to study in college and who to date. Without question, many of those decisions would have been different if I didn’t have EODD.
Don’t just assume that your child is negative, apathetic, anti-social and lacking in ambition. It’s possible that EODD has been a part of his life so long that the symptoms have woven themselves into your (and their) perception of his personality. If your child has been exhibiting any of the symptoms of depression, even in a milder form, it is crucial that you consult a professional.
2 Comments
Fabian
I have a hard time finding articles about this topic.
I just found out, at 32, that I had this all my life.
Why isn’t anyone ending these articles with how their respective state is now?
WHAT HAPPENED?
Are you better? Did treatment help? What treatment?
I have a psychiatrist’s appointment next Tuesday and no clue what my prospects are.
Deborah
I’ve been on antidepressants since I was diagnosed at 27. I had success with the first antidepressant I was put on, which is an old one called Norpramin. I switched to Wellbutrin after about 10 years. I have had some trouble since hitting menopause, but a problem unique to women of my age.
If you have dysthymia and are not currently experiencing an episode of major depression, the psychiatrist could recommend cognitive behavioral therapy as the sole treatment. I would also add that stress exacerbates depression, so you should do your best to de-stress frequently, either with exercise, meditation, or both. Make sure your diet is nutritious and that you aren’t deficient in any vitamins or minerals. Also make sure that you don’t isolate yourself, as human contact seems to be beneficial for depression.